The intestine-brain axis in the case of neurocognitive disorders
Studies have long demonstrated an important correlation between alterations of the intestinal microbiota – detectable by the analysis of feces and urine – and diseases of the psychiatric sphere, neurocognitive and mood disorders, in particular depression but also migraine, anxiety, insomnia. One line of study is precisely that which is dedicated to understanding how the microbiota can influence the metabolic process of tryptophan and the synthesis of serotonin, and how a dysfunction in the serotonergic mechanism can be considered one of the main risk factors of depressive syndromes in adults.
So let’s go back to talking about the intestine-brain axis and recover those concepts that allow us to understand why the health of one is deeply connected with the health of the other.
The metabolism of tryptophan at a glance
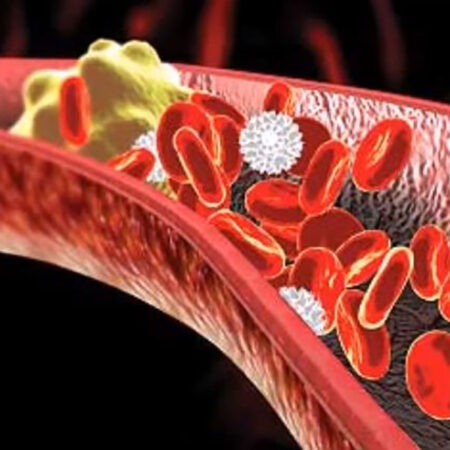
Tryptophan (TPH) is absorbed in the intestine as an essential amino acid; once in circulation, most of it is destined for the cells for protein synthesis, a part is absorbed through the enterochromaffin cells which use it for the synthesis of serotonin, the remainder is catabolized through the kynurenine degradation process.
During this last step, however, the production of kynurenic acid, a protective substance for the body, or that of quinolinic acid, which, as we have seen in a previous article, can be transformed into a neurotoxin, capable of to induce wide-ranging inflammatory states.
Attention: pathological states and physical imbalances can influence, or be influenced by, the bioactive metabolites of pro-inflammatory tryptophan, which in turn, if in large quantities, are considered risk factors for many diseases and/or internal inflammatory conditions including including irritable bowel syndrome (IBS), neurodegenerative and cerebrovascular diseases.
In particular, quinolinic acid is perhaps the most dangerous metabolite of tryptophan, because it is able to reach the brain and its vascular system. It is said that, once produced, it must “forcefully” turn into a threat, because under normal conditions astrocytes – a type of neuron in the brain – are able to neutralize it.
However, when there is a chronic dysregulation of the entire degradation process of tryptophan and its metabolites, the quinolinic acid remains in circulation and induces the early death of cellular mitochondria (tiny organelles in which the energy needed by the body is produced to perform its primary and secondary physiological functions).
Too much circulating quinolinic acid (and too little kynurenic acid, its “good” antagonist), can lead to:
Increased production of free radicals with oxidative action on all cells of the body (this leads to premature aging and vulnerability to disease)
Concomitant reduction of free radical scavenging enzymes
Impaired cellular respiration process, resulting in loss of energy and general weakening
Irreversible damage to cell mitochondrial membranes
Multiple factors contribute to messing up tryptophan metabolism and can, therefore, negatively affect serotonin synthesis.
Therefore, in case of unstable mood, exhaustion, memory difficulties, recurring migraine, it is advisable to make sure that there is no intestinal dysbiosis problem. If so, the resolution of dysbiosis, through a joint approach between diet and nutraceuticals, will allow an improvement of all metabolic reactions including those relating to tryptophan metabolism.
What we recommend you do to know if you have a tryptophan/serotonin gap
Through the analysis of organic acids, from a urine sample, we can provide the specialist with quantitative evidence to understand if we have enough serotonin for our needs and beyond. Through this test it is possible to identify the presence of states of chronic sub-inflammation caused by an altered tryptophan metabolism and an abnormal production of quinolinic acid.