What happens before and after the blood transport of cholesterol, triglycerides and other lipids
The metabolism of dietary fats is a complex process, which takes place in different organs of our body. First of all, since we are talking about insoluble substances, the lipids ingested through food will be diluted and transformed into assimilable compounds. This operation takes place in the small intestine, it is called emulsification and it is carried out by bile salts and some pancreatic enzymes.
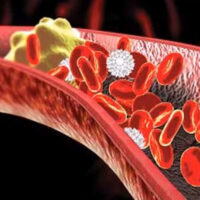
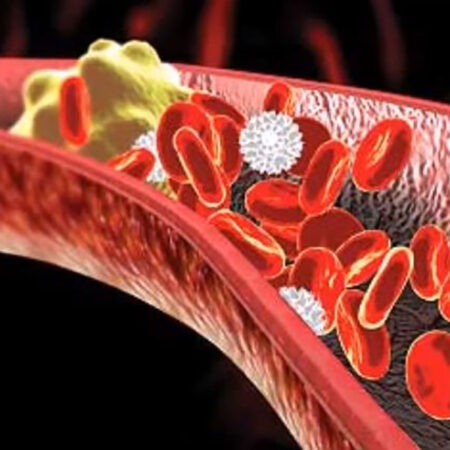
Once digested, the lipids first flow into the lymphatic vessels, and from these into the blood, where they are directed towards their main destinations conjugated to lipoproteins. The bulk of total dietary lipids, as already specified, is made up of triglycerides, which must be stored in adipose tissue, unless they are needed immediately if the body does not have sufficient quantities of glucose available.
Returning to lipoproteins, they change depending on the lipid they transport, and whether this is exogenous or endogenous. Let’s see the main ones that we can find in our blood with their acronyms:
- Chylomicrons: exclusively transport dietary triglycerides from the intestine to the tissues in which they must be stored.
- VLDL (Very low density lipoprotein): transport endogenous triglycerides, i.e. those synthesized by the liver to the destination tissues. These lipoproteins contain a small percentage of esterased cholesterol.
- IDL (Intermediate low lipoprotein/medium density lipoprotein): VLDL particles that have partially exhausted their quota of triglycerides. These lipoproteins are precursors of LDL.
- LDL (Low density lipoprotein): IDL particles emptied of triglycerides and with a high percentage of esterased cholesterol.
- HDL (High density lipoprotein): they collect excess cholesterol present in the tissues and transport it to the liver or to other cells that require additional cholesterol levels.
Lipoproteins, therefore, are essential for the transport of lipids. But what happens before and after this blood “journey” of cholesterol and triglycerides, and other lipids?
Fatty acid metabolism and catabolism
Fatty acids, which as we have seen are the non-soluble part of triglycerides and are composed of more or less long chains of carbon atoms with bonds, or without bonds. Once introduced into the blood and transported by lipoproteins, fatty acids must be absorbed by the cells and enter the mitochondria, passing their membranes through a reaction called the carnitine shuttle, in which COA (acetyl-coenzyme, a molecule synthesized by the mitochondria itself) comes into play. starting from pyruvate, itself a derivative of dietary glucose), and carnitine (an amino acid). Once they enter the mitochondria, fatty acids are subjected to beta-oxidation, a catabolic process that serves to release energy by breaking carbon bonds, and which takes place in four enzymatic reactions. In fact, it happens that during beta-oxidation two carbon molecules are released, which, transforming into Acetyl-CoA through the Krebs cycle, generate energy.
Also during beta-oxidation, the molecules NADH and NADH2 are released which are also used to produce energy during the electron transport chain. This complex sequence of biochemical reactions occurs in all cells of the body that contain mitochondria (and therefore not in blood cells, which have no nucleus), with the exception of brain cells, where fatty acids cannot reach. When dysfunctions occur at the beta-oxidation level, as happens in the case of specific genetic pathologies or metabolic diseases including diabetes, this happens because the enzymes necessary for the breakdown of lipids are missing, or the body does not have sufficient reserves of carnitine, and then we go into an energy deficit. This condition involves the activation of alternative fatty acid degradation pathways, including omega oxidation, which is not normally a “used” pathway.
Again in the case of alterations in the beta-oxidation process of fatty acids, an abnormal production of ketone bodies can occur – as happens in the case of fasting or in pathologies such as diabetes. In fact, ketogenesis, which takes place in liver cells, is a process that depends on the beta-oxidation of fatty acids because it exploits the acetyl-CoA produced by this pathway. Once produced by the liver, the ketone bodies move from this organ to be transported elsewhere, via the blood, and reconverted into energy again (ketolysis). The excessive and harmful production of ketone bodies can also be “measured” in urine.
Glycerol metabolism
Glycerol is, as we have seen, the water-soluble component of triglycerides, and therefore easily assimilable. Since it is a sugar, once it reaches the mitochondria, it is used in the glycolysis process, exactly like the glucose of carbohydrates, for the production of energy, i.e. ATP (the “energy control unit” of the cells) during the transport chain of electrons. Glycerol metabolites are also used for the endogenous synthesis of triglycerides.
Metabolism of ketone bodies
When we talk about fats that the body uses in place of glucose for energy, we are talking about ketone bodies or ketones. Normally only a small part of “small” energy – that necessary for routine biological functions – is obtained from the lipids stored in adipose cells.
But in some cases: low carb slimming diets (with low carbohydrate consumption, also called, not surprisingly, ketogenic diets), significant physical effort, diabetes, this production increases. The liver is always responsible for the synthesis of ketone bodies – which are water-soluble molecules. Ketones are reserve fats that are processed to overcome the brain’s blood barrier and also be used by brain cells.
HDL cholesterol metabolism
As anticipated, HDL are protein particles that are produced by the liver. Originally, therefore, they are “empty”, but they receive any excess cholesterol from LDL and the body’s cells, and then send it back to the liver, or to the steroidogenic cells, which use it to produce steroid hormones (for example estrogens and testosterone), or bile salts. It is essential for our cardiovascular health to have a good production of HDL, so that excess cholesterol does not remain in circulation and form atherosclerotic plaques on the venous and arterial walls.